What does it take to implement EUS in our center?
The integration of endoscopic ultrasound (EUS) capabilities into ambulatory surgery centers (ASC) represents a significant opportunity for facility growth, enhanced patient care, and improved financial outcomes. Historically, numerous barriers, including high equipment costs and specialized training requirements, have confined EUS procedures to academic hospitals, tertiary care centers or both. This limitation has restricted patient access to this valuable diagnostic and therapeutic modality. In the past few years, physicians, administrators, and owners have seen the value of EUS in the ASC; and because of some of today’s product breakthroughs, it is even more appealing.
This white paper provides ASC leaders, physicians, and administrators with a comprehensive roadmap for successfully implementing EUS in the ASC. With recent technological advancements resulting in cost efficiencies, ASCs now have unprecedented opportunities to incorporate these procedures efficiently and profitably.
The following guide addresses critical implementation aspects, including:
- Financial considerations and return on investment
- Equipment and technical requirements
- Patient selection criteria
- Staff training and responsibilities
- Billing and reimbursement strategies
- Operational best practices for success
The Economics of EUS in ASCs: Understanding what it can bring to your ASC
Potential Costs:
Capital expenditures have traditionally confined EUS procedures to hospital settings with higher procedure volumes and larger capital budgets. This limitation has created accessibility gaps for patients who could benefit from these procedures in the more convenient, preferred, and often more cost-effective ASC environment.
Implementing EUS in the ASCs has been expensive (see Table 1). Traditional ultrasound scanners cost $200,000+, multiple specialized echoendoscopes at $80,000+ each, dedicated service costing $10,000 have all amounted to about $400,000 total, with a significant investment in that first year, often totaling more than $250,000.
In contrast, the innovative EndoSound Vision System™ (EVS™) offers a fully functioning EUS system with a highly portable ultrasound scanner and capital equipment at significantly lower cost ($50,000) (Table 1). The EVS does not have an annual service contract and there are no expensive echoendoscopes to purchase.
| Component | Traditional Systems | EVS |
| Processors/Scanners | $200,000+ | $50,000 |
| Echoendoscopes | $80,000 each (minimum 2 needed) | Converts existing endoscopes |
| Annual Service | $10,000+ per scope per year | Reduced maintenance costs |
| Training | Extensive specialist training | Personalized training service |
Potential Revenue:
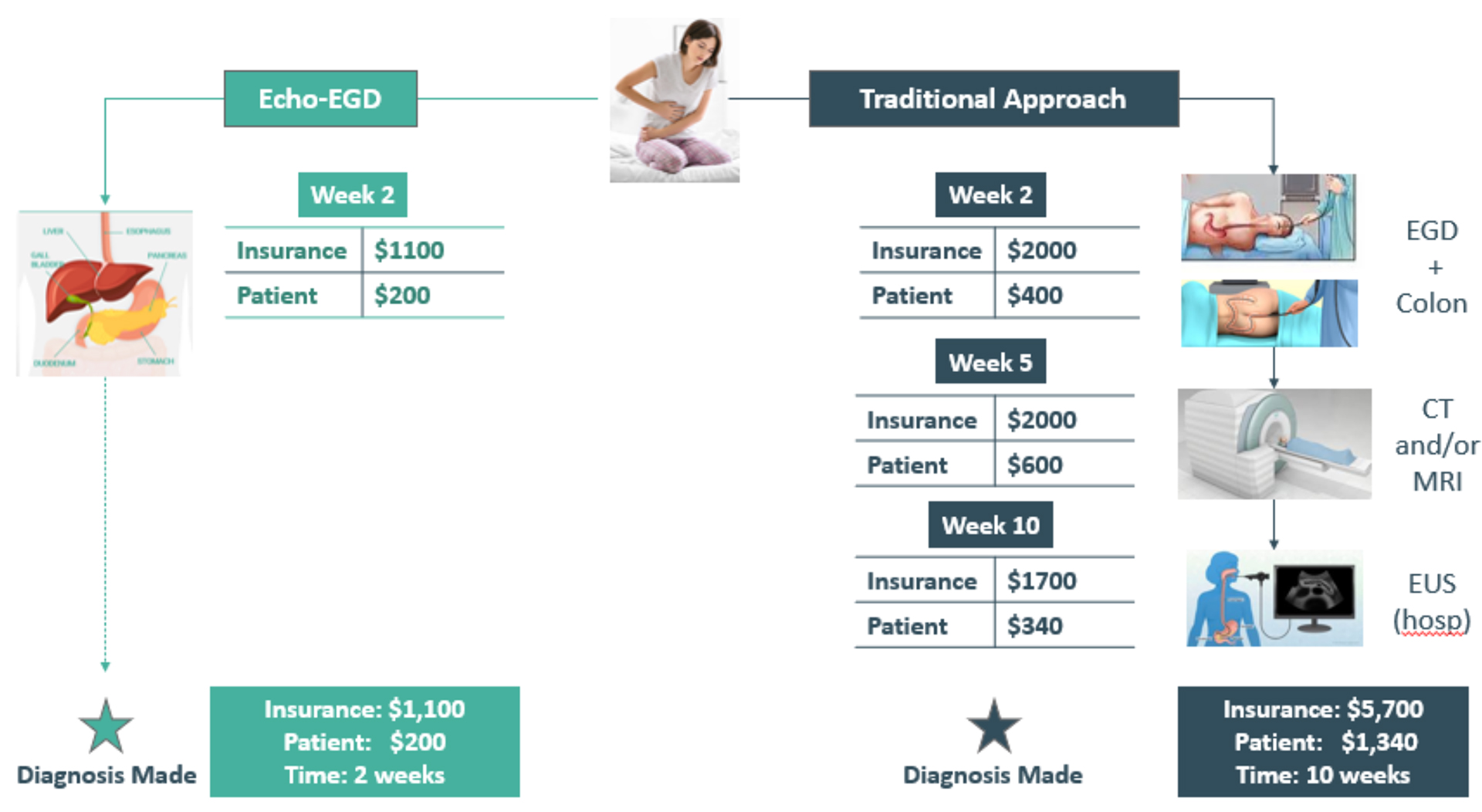
One aspect of the financial picture is the amount of reimbursement for EUS versus EGD. Simply compared, EUS procedures, on average, reimburse $864* per Medicare case; standard EGDs reimburse $503* per Medicare case. The potential to almost double procedure revenue is clear.
For many facilities, the revenue potential extends beyond these base numbers when considering:
- Private payer rates: Typically, higher than Medicare rates, often by 15-30%
- Transitional Pass-Through (TPT) payments: Additional reimbursement for innovative devices (which the EVS has for its disposable component)
- Reduced referral leakage: Retention of patients who would otherwise be referred to hospitals
- Increased physician satisfaction: Enhanced recruitment and retention of specialists
- Market differentiation: Competitive advantage over other ASCs in the region
ASCs implementing EUS with newer, more cost-effective technologies like the EVS can typically expect initial investment recovery quicker, long-term revenue enhancement, operational efficiencies, maintaining optimal cash flow and predictable financial planning.
Technical Requirements
With EUS in your ASC, understanding the equipment, room, and staff requirements are crucial. To date, it has been a burden to get EUS in the ASC because the equipment has been bulky and big, and not easily transportable. Endosound and EVS solve these issues (see below) and make preparation to perform EUS in your ASC seamless.
Start with acquiring an EUS system, including an ultrasound processor and compatible echoendoscopes. You’ll need at least two scopes: linear echoendoscopes and potentially FNA and FNB needles. Look at several systems and their costs. Remember, the EVS was designed with this distinct price burden in mind. Moreover, you will convert your existing gastroscopes into EUS-capable devices. The EVS is a portable system (easily moved between rooms) that works with your current equipment, and our probe eliminates the need for multiple specialized scopes.
Allocate a dedicated room with adequate space for ultrasound equipment and monitors. Verify proper electrical and network connections. Just like your reprocessing for current scopes, the EUS scopes will follow similar protocols. For the EVS, its footprint is smaller than existing EUS systems, and the probe (UTM) has a simplified reprocessing protocol (no working channel means easier, safer cleaning). Lastly, and importantly, we train your staff on EUS-specific equipment, procedures, and staff responsibilities during the procedure, and cleaning and reprocessing. With our highly experienced and dedicated team, we’ll be with you every step of the way.
Reimbursement, Billing and Add-On payments
Even though you know this well, when billing for endoscopic procedures in ASCs, facility fees cover several key elements:
- ASC facility usage (operating rooms, recovery areas, waiting rooms)
- Services from nurses and technical staff
- Drugs and biologicals not separately paid under OPPS
Physicians bill their professional services separately through consultations, evaluations, and follow-ups. ASCs use CPT and HCPCS Level II codes, with payments typically calculated as a percentage of hospital rates.
Maximizing Reimbursement Success
For optimal reimbursement:
- Review private payer contracts thoroughly
- Ensure EUS procedures are included in the contract language
- For multiple procedures, remember the first is billed at full rate, with subsequent procedures may be reduced by 50%
- Maintain compliance with all billing regulations
- Implement pre-authorization processes for high-value procedures and develop a process for claims denials
Specific Codes for EUS and the EVS
When billing specifically for EUS procedures, including the EVS, there are several CPT codes.
| CPT Code | Description |
| 43231 | Esophagogastroduodenoscopy with endoscopic ultrasound examination |
| 43232 | Esophagogastroduodenoscopy with endoscopic ultrasound examination and fine needle aspiration |
| 43237 | Endoscopic ultrasound examination, esophagus, stomach, and duodenum |
| 43238 | Endoscopic ultrasound examination with fine needle aspiration, esophagus, stomach, and duodenum |
| 43242 | Endoscopic ultrasound examination, pancreaticobiliary with fine needle aspiration |
| 43253 | Endoscopic ultrasound-guided transmural injection |
| 43259 | Endoscopic ultrasound examination of esophagus, stomach, and duodenum |
| 43240 | Esophagogastroduodenoscopy with transmural drainage of pseudocyst |
Transition Pass Through Payment Code – Additional Reimbursement Opportunity
The EVS received a Transition Pass Through (TPT) payment code from CMS in July 2024. The TPT code, C1606, provides additional reimbursement for the disposable component of the EVS under the Medicare Hospital OPPS and ASC Payment System.
This specialized pathway is designed to adequately compensate healthcare facilities for the cost of adopting cutting-edge technologies like EVS, allowing for an add-on payment along with the standard CPT codes.
This additional payment has been important for new centers evaluating EVS and is exclusively tied to the EVS.
Preparing Your ASC and Staff for Successful EUS Implementation
To ensure your staff and center are well-prepared for EUS procedures, here are some key insights the EndoSound team has gathered during installations across the US and Latin America.

Establishing a True Partnership
While “partnership” is often used to describe industry-center collaborations, implementing EUS in your ASC requires genuine open dialogue. True partnership means both parties have a shared investment in your program’s success, making communication essential. At EndoSound, our risk-sharing partnership is the first of its kind.

GI Tech Development
Training ASC technicians without EUS experience is essential for them to reach the proficiency level of their hospital counterparts. We train techs on the EVS and in collaboration with our clinicians, the basics around EUS. Our team is present during the entire installation and always available when called upon post installation.

Billing Resource Assistance
Your industry partner should offer support with appropriate procedure codes and share reimbursement insights from other facilities. This collaborative approach helps your billing department navigate coding, reimbursement pathways, and payer contracting more effectively. EndoSound involves health economic experts to assist our clients and will introduce prospective centers to reference customers regarding this process.

Ongoing Expert Support
Implement direct communication channels with your industry partner that extend well beyond initial installation. Whether through phone calls or video conferencing, this continuous access provides critical support during pre-procedure preparation, procedural questions, and post-procedure evaluation. Your industry partner should be committed to a long-lasting partnership that goes beyond initial installation.
Conclusion: The Future of EUS in the ASC Setting
The integration of EUS into the ASC environment represents a significant advancement in patient care, clinical capability, and business opportunity. With innovative technologies like the EVS reducing traditional barriers to entry, ASCs now have unprecedented access to this valuable diagnostic and therapeutic modality.
By following the comprehensive roadmap outlined in this white paper, facilities can navigate the implementation process successfully, avoiding common pitfalls while maximizing clinical and financial outcomes. Key factors that will lead to success include:
- Thorough planning and preparation
- Investment in staff development and training
- Strategic partnerships with vendors and healthcare institutions
- Attention to reimbursement and billing
As healthcare continues to shift toward value-based models and patient-centered care, the ability to offer advanced procedures like EUS in convenient, cost-effective settings is increasingly important. Early adopters of these capabilities will be well-positioned to lead in this evolving landscape, providing enhanced care while building sustainable competitive advantages.
About EndoSound
EndoSound offers a revolutionary system that transforms standard endoscopes into EUS devices, improving patient care while reducing healthcare costs. The EVS is designed to address the historical barriers to EUS implementation in the ASC setting, making this valuable technology accessible to more facilities and patients.
Learn more at www.endosound.com or call (971) 231-4791. Headquartered in Portland, OR.
This white paper is intended for informational purposes only and does not constitute medical, legal, or financial advice. Healthcare facilities should consult with appropriate professionals regarding specific implementation questions.