The Evolution and Promise of Echo-EGD: Enhancing Standard Endoscopy with Ultrasound
When a patient presents with abdominal pain or dyspepsia, physicians may choose from a variety of diagnostic tests to uncover the underlying cause. While standard EGD (esophagogastroduodenoscopy) is frequently utilized, Echo-EGD, which enhances traditional endoscopy with ultrasound, holds the promise of greater diagnostic accuracy. It should be noted that Echo-EGD is distinguished from typical EUS indications, namely abnormalities noted on prior endoscopy or imaging for further evaluation.
The choice between standard EGD and Echo-EGD depends on the indication. The follow-up and/or evaluation of lesions such as Barrett’s, gastric ulcers, etc. are common EGD indications. However, there is also significant overlap i.e. patients referred for diagnostic evaluation of abdominal pain or dyspeptic symptoms which there is a significant percentage of patients. Of the 8 million EGDs performed annually in the United States, many patients could fall into the diagnostic category and could benefit from the enhanced visualization that Echo-EGD provides. Indeed, many of these patients come to EUS after EGD and other diagnostic testing has been uninformative.


Figure 1. (a) Illustration on left is of organs seen with standard EGD. (b) Illustration on right is of organs examined with Echo-EGD. This comprehensive view can improve diagnostic accuracy and potentially reduce the need for follow-up imaging.
Compelling Clinical Data
Echo-EGD is not a new concept. There are significant data dating back to 2000 showing clinical benefits (Table 1). Echo-EGD has not been widely adopted, primarily due to the high costs of traditional endoscopic ultrasound (EUS) systems and their limitations in the hospital setting. However, with new technology like the EndoSound Vision System™ (EVS™), which can convert any endoscope into an EUS device at a lower price point, Echo-EGD has become more feasible.
| Title | Authors and Reference | Implications for Echo-EGD (EE) |
| EUS to detect evidence of pancreatic disease in patients with persistent or nonspecific dyspepsia | Sahai et al., Gastrointest Endosc 2000;52:153-9. | EE demonstrated that 40% (51/156) of dyspepsia patients had evidence of pancreatic disease |
| An assessment of the potential value of endoscopic ultrasound as a cost-minimizing tool in dyspeptic patients with persistent symptoms | Sahai et al., Endoscopy 2001; 33: 662–667 | Dyspepsia evaluation had a lower cost with EE based approach |
| EUS in the management of uninvestigated dyspepsia | Lee et al., Gastrointest Endosc 2002; 56: 842–848 | EE changed management in 25% of dyspepsia patients |
| EUS compared with endoscopy plus transabdominal US in the initial diagnostic evaluation of patients with upper abdominal pain | Chang et al., Gastrointest Endos 2010; 72: 967-74 | 38% of patients with upper abdominal pain had a diagnosis made (66/172) (38%); of those 48% were EE based
|
| Endosonography For Right-sided and Acute Upper Intestinal Misery: the EFRAIM study | Jung et al., United European Gastro Journal 1(5) 329–334 | 223 patients with abdominal pain. EE had a higher diagnostic yield than the combination of transabdominal US and EGD (62.3 vs. 50.7%; p = 0.001). |
Table 1. Echo-EGD clinical publications
Why Echo-EGD Matters
- In the US approximately 8 million standard EGDs are performed annually
- Many of these are performed for diagnostic indications (e.g. abdominal pain, and/or dyspepsia) and these patients could benefit from the enhanced diagnostic capabilities where pathology was identified in as many as 35% of patients (Sahai et al., 2000).
- Clinical evidence suggests that Echo-EGD as a first line diagnostic could be more effective in discovery of disease or the causes of the patient’s presentation.
- Lastly, the procedure can be safely performed in ambulatory surgical centers (ASCs), and because of the introduction of the EVS, access to care can be improved and costs are reduced.
Echo-EGD: Time and Money
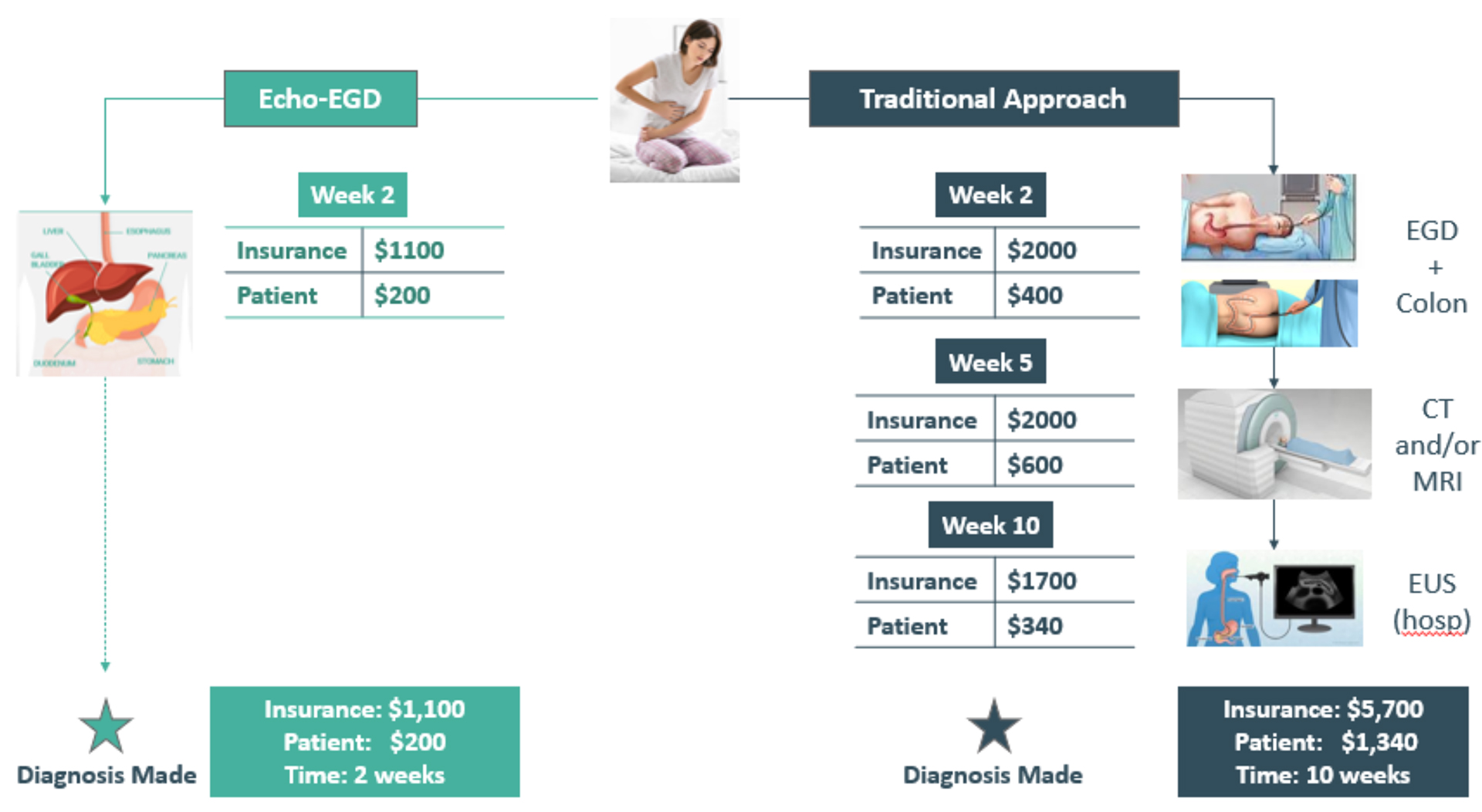
Figure 2. Comparison between patient flow on right with standard EGD first and Echo-EGD on left side. Both time and money are saved with Echo-EGD.
When a patient comes in with abdominal pain and/or dyspepsia, they face two potential diagnostic paths – and the difference in both time and money is striking.
Standard EGD (“Traditional Approach”) (Figure 2 right side), often involves a multi-step diagnostic journey:
- Week 1: Patient presents with upper abdominal pain
- Week 2: Initial EGD (Insurance cost: $2,000, Patient cost: $400)
- Week 5: Additional imaging like CT or MRI (Insurance cost: $2,000, Patient cost: $600)
- Week 10: Hospital-based EUS (Insurance cost: $1,700, Patient cost: $340)
The standard EGD patient flow may stretch over 10 weeks, with total costs reaching $5,700* for insurance and $1,340* for the patient. The process requires multiple appointments, procedures, and recovery periods.
With Echo-EGD (Figure 2, left side), patients can benefit because it offers a streamlined diagnostic process. After the initial presentation of upper abdominal pain, by week 2, patients can receive a comprehensive examination that costs insurance $1,100 and the patient just $200. Clearly a more simplified path. This single procedure combines traditional endoscopy with ultrasound imaging, leading to a diagnosis within two weeks. Total cost: $1,320.*
The Bottom Line
In this example, the difference is clear – Echo-EGD saves:
- 8 weeks of diagnostic time
- $4,600 in insurance costs
- $1,120 in patient out-of-pocket expenses
- Multiple medical visits and procedures
These numbers are based on CMS national averages and are likely much higher for private payers. Finally, this change in patient flow has the potential to reduce healthcare costs and improve patient’s lives.
Beyond the numbers, this represents less time spent uncertain, fewer medical procedures, and a more efficient path to treatment for patients seeking answers about their health.
As noted by Dr. Leonardo Sosa at IHU de Strasbourg, France, in his textbook titled Pancreatic Endoscopic Ultrasound: Current Practice and Clinical Applications 1st Edition, he states that the EVS is a:
“new and revolutionary upper endoscopy solution [that] offers the promise of “democratizing” internal sonography while performing EGD, making Echo-EGD [or Echo-Endoscopy] widely available to all patients with upper digestive symptoms. One could imagine a time when internal sonography will maximize the diagnostic yield of every upper endoscopy, providing visualization of luminal features and at the same time, adjacent, extra-luminal structures. This new device will probably increase the number of second-intention EUS worldwide for precision diagnostics and it will compete with tomography and abdominal ultrasound.”
The EVS enables physicians to perform Echo-EGD in the ASC, making this powerful diagnostic tool accessible to all patients with upper digestive symptoms. This innovation could transform standard endoscopy patient pathways by integrating enhanced imaging earlier in the diagnostic process. Revised clinical algorithms that incorporate Echo-EGD more frequently can deliver significant benefits to all stakeholders—reducing diagnostic timelines for patients, lowering overall healthcare costs for insurers, and creating more efficient workflows for providers.
*Cost estimates based on CMS, Google search. Actual costs could be higher or lower in your state and clinic.